Users Who Spiked
GROUP B STREPTOCOCCUS IN NEWBORNS
Private Notes
Private Notes
Notes
Abstract
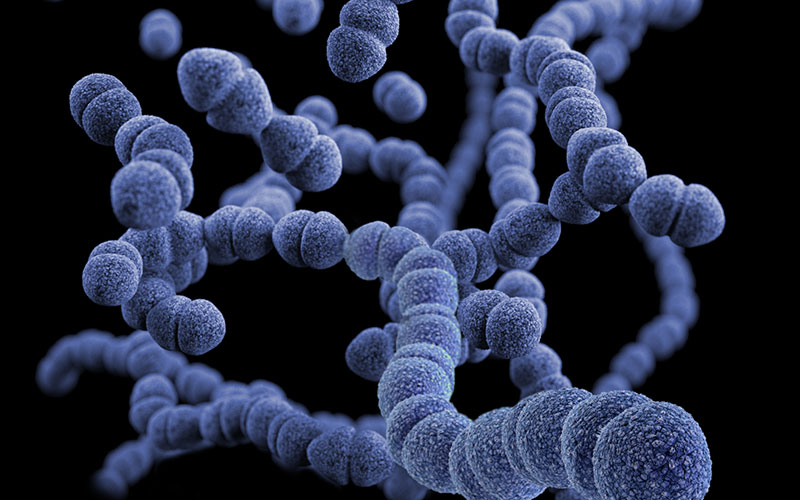
This paper describes the prevention techniques, symptoms, effects and risk factors that result in the death of infants due to the colonization of the bacterium Streptococcus agalactiae. More commonly recognized as Group B Streptococcus (GBS), it is a leading cause in infant mortality rates (Anonymous 2011). Although there is no definitive cure recent research has identified how the bacteria evades the maternal immune system (Vornhagen 2016). Despite this new research the disease continues to kill newborns at a rate of 4-6% (Anonymous 2016). Time of membrane rupture during birth (water breaking), as well as premature birth (before 37 weeks) can increase the risks of a newborn GBS infection, which without treatment can be detrimental (Dekker 2013). Treatment during labor has shown to be effective, although it comes with its own risk of complications to the newborns normal healthy microbiota (Fouhy et al 2012).
Group B Streptococcus in Newborns
How the Bacteria Evades Immune Defenses
Hyaluronidase is an enzyme that the strain Streptococcus agalactiae produces in the vaginal canal that allows it to avoid detection by the body's immune system. The hyaluronidase neutralizes and blocks the naturally occurring hydraulic acid present in the vaginal canal. (Vornhagen 2016). Finding the source to the infection is the beginning of developing a cure.
Risk Factors and Prevention
GBS is a prevalent asymptomatic infection among women- about 25% carry the bacteria with no apparent symptoms resulting in dangerous possibilities. (Anonymous 2011). Certain factors can increase a woman's chances of passing on the infection to her unborn child during birth. In children GBS causes fever, difficulty breathing and a lack of activity. If untreated it can cause an infection of the blood and even death. (Dekker 2013). If the baby survives the infection then he can develop mental, hearing and vision problems later on in life due to the severity of the infection. (Anonymous 2011). Common risk factors that are of high concerns are developing a fever during labor, water breaking long before the child is born and delivering a child less than 37 weeks into the pregnancy. (Adair et al 2003). Fortunately doctors in coordination with the Centers for Disease Control and Prevention (CDC) have started to implement screening that allows for the prevention of infection during birth. (Anonymous 2016).
The CDC have started a universal screening for pregnant women 35-37 weeks into pregnancy to test for the GBS strain. This testing is done by swabbing the expecting woman's vaginal and rectal canal with a cotton swab and sending the culture to the lab for 48 hours. Typically this test is about 91% accurate and the appropriate measures can be given to the mother during birth. (Dekker 2013). Penicillin is the most common drug given to women during birth via IV. It is given during birth due to the bacteria's ability to grow back quickly. This antibiotic treatment helps to kill a large majority of the bacteria that could affect the infant as it passes through the birth canal. (Anonymous 2016). Despite efforts to prevent infection, some newborns are still born with the disease and must be treated after birth.
Treatment of the Newborn After Birth
On the onset of symptoms such as fever, lethargy, blueish color to the skin, difficulty breathing or feeding a newborn infant should have sterile body fluids tested for the GBS bacteria. The blood or spinal fluid is then sent to a lab where the sample is cultured for several days to confirm diagnosis. Once a diagnosis has been confirmed the baby will then receive penicillin or a similar antibiotic through an IV to avoid further complications. (Anonymous 2016). Mothers treated for the disease during labor will have their infants tested shortly after birth and one week out. Unfortunately mothers who were not treated for the infection must wait until symptoms develop physically before having their baby tested. Although the alternatives are worse there are negative effects of the antibiotics given to newborns to offset the disease.
Negative Risks of the Treatment of Newborns
In Fouhy et al. (2012) they studied infants that received antibiotic treatment within 48 hours of birth and healthy infants that had not received the medication. Overall they found that the infants who had received the drugs had a lower colonization of healthy bacteria a few months later. This is significant because the bacteria of the intestines- the healthy kind- can help the body resist infection from unhealthy bacteria by creating a competitive environment. This affects infants with cured GBS. Ampicillin, a penicillin antibiotic, was used in the study (Fouhy et al 2012) and the correlation between antibiotics and low normal biota of the intestinal tract has dangerous risks. Without those bacteria colonizing the intestines this could lead to more infections later on.
Conclusion and Future Study
Although the research has now presented a reason behind the infection occurring but has yet to produce a viable vaccination to prevent the bacteria from colonizing completely. Once a vaccine has been developed the antibiotic treatment during birth or after birth can be eliminated and therefore reduce the risk to the infant.
References
Adair, C. E., Kowalsky, L., Quon, H., Ma, D., Stoffman, J., McGeer, A., Davies, H. D. (2003, August 05). Risk factors for early-onset group B streptococcal disease in neonates: A population-based case-control study. Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/12900477
Anonymous. (2011, February 08). Group B Strep in Newborns. Retrieved from https://www.cdc.gov/healthcommunication/toolstemplates/entertainmented/tips/strep.html
Anonymous. (2016, May 23). Group B Strep Infection in Newborns. Retrieved from https://www.cdc.gov/groupbstrep/about/newborns-pregnant.html
Dekker, R. (2017, February 15). Group B Strep in Pregnancy: Evidence for Antibiotics and Alternatives. Retrieved from https://evidencebasedbirth.com/groupbstrep/
Fouhy, F., Guinane, C. M., Hussey, S., Wall, R., Ryan, C. A., Dempsey, E. M., . . . Cotter, P. D. (2012, November). High-Throughput Sequencing Reveals the Incomplete, Short-Term Recovery of Infant Gut Microbiota following Parenteral Antibiotic Treatment with Ampicillin and Gentamicin. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3486619/
Vornhagenab, J., Quach, P., Boldenow, E., Merillat, S., Whidbey, C., Ngo, L. Y., Rajagopal, L. (2016, June 28). Bacterial Hyaluronidase Promotes Ascending GBS Infection and Preterm Birth. Retrieved from http://mbio.asm.org/content/7/3/e00781-16.full#ref-list-1























